Chronic kidney disease is a progressive loss of renal function over a period of months or years , and characterized by abnormally low and deteriorating glomerular filtration rate (1). Individuals with glomerular filtration rate<60 ml/min/1.73 m2 for three monthsare classified as having chronic renal disease.End stage renal disease has highest prevalence of dermatological manifestations (50-100 % cases)
Common causes of chronic kidney disease in India are diabetes, hypertension &structural kidney defect. The prevalence of chronic renal failure is increasing in India.
Skin being an external organ is often a window to the progressive pathology going on in kidneys.
There are various skin manifestations in chronic kidney disease which can be specific or non-specific
Pathomechanism of dermatological changes-
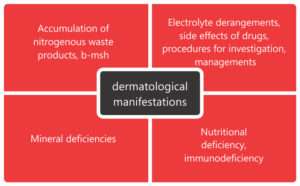
The commonly seen dermatologic manifestations are-
Cutaneous changes-xerosis, pruritus ,pigmentation abnormalities including pallor and grey-brown pigmentation,perforating disorders ,superficial infections, purpura&ecchymoses.
Nails –half and half nails,leukonychia,pitting,beau’s lines,splinterhaemorrhages, absence of lunula,red lunula,koilonychia
Hairs-thin and lusterless scalp hairs,telogen effluvium,hypertricosis in patients on cyclosporine.
Mucosa-xerostomia, uremic mucositis,bald tongue,pigmentation of mucosa,macroglossia with increased teeth markings,candidiasis,gingivitis,periodontitis.
The cutaneous manifestations related to hemodialysis include changes at A-V fistula site, xerosis, pruritus &pseudoporphyria
Non-specific changes-
1.Xerosis-
Xerosis is seen in 50-85% of patients of CKD.It is attributable to atrophy of sebaceous glands sudoriferous glands and volume depletion secondary to diuretics(3). Xerosiscan be treated by applying moisturizers with 5-10 % urea and 2-3% salicylic acid.
2.Pigmentary abnormalities-
a.Pallor-pallor is seen due to anemia of chronic disease
b.Yellowing of skin –yellowing of skin is due to retention of fat-soluble pigments in the dermis and subcutaneous tissue, such as carotenoids and urobilinogen
c.Grayish-brown skin-greyish brown pigmentation is seen due to the deposit of hemosiderin;
d.Hyperpigmentation associated with sun exposure
e.Ecchymosis-ecchymoses are seen secondary to platelet dysfunction
3.Pruritus
The pathophysiology of pruritus lies in xerosis,hyperparathyroidism and hypervitaminosisA,iron deficiency anemia and electrolyte imbalance.. Therapeutic modalities tried are-antihistaminics, ondansetron, serotonin antagonists,activated charcoal, cholestyramine, optimizing daily and in severe cases by narrow band UV-B & UV-A phototherapy.
4.Gynecomastia –
It is seen in males due to increase in prolactin level
5.Purpura-
They are seen secondary to defects in platelet function and use of heparin during dialysis.
6.Nail changes-
Nail changes associated with chronic kidney disease include –
a.Koilonychia-
Ridged nails that are spoon shaped & concave due to anemia of chronic disease and decreased erythropoietin levels in chronic renal failure.
b.Absent lunula-
Absence of visible portion of white matrix. It reflects metabolic disorders andanemia.

Specific manifestations-
1.Perforating disorders-
They are disorders of trans-epidermal elimination of altered keratin or dermal connective tissue material . These disorders include- perforating folliculitis , Kyrle’s disease,elastosisperforansserpiginosa and reactive perforating collagenosis(4,5).Clinically, the lesions are hyperkeratotic to verrucouspapules ,umbilicated nodulesor plaques over extremities with central keratotic plug. There is no effective treatment for perforating disorder,but topical retinoids,allopurinol,UVB,PUVA have been tried.

2. Calciphylaxis-
Poorly understood and highly morbid syndrome of vascular calcification and skin necrosis ;seen in stage 5 of chronic kidney disease. Lesions first present over lower extremities,abdomen,buttocksand penis as areas of mottling of skin & induration in a livedoreticularis pattern . The progression is very rapid leading to formation of ulcerated,gangrenous lesions.Prognosis is very poor in untreated patients with ulceration , with mortality rate of 60-80 %. It can be treated by cincalcet,sodium thiosulphate and surgical debridement for ulcerated lesions.
3. Nephrogenic systemic fibrosis (NSF)-
Scleroderma like changes in skin and internal organs in patients of CRF exposed to gadolinium based contrast agents.
4. Half and half nails-
It is characterized by a proximal whitish band and distal brownish or pinkish discoloration. The pathogenesis is attributed to an increase of the melanocytic stimulating hormone and increase in capillary number and thickness.

5. Uremic frost-
One of the rarest presentations is uremic frost, seen in only 3% of the patients with ESRD. It is related to frank uremia and recognized as a white deposit on the skin, secondary to crystallized urea excreted in sweat.
6. Bullous disease of dialysis –
Bullous lesions on photoexposed parts of end-stage renal failure resembling lesions of porphyria cutaneatarda.The porphyrin levels are normal or mildly raised.
7. Arterial steal syndrome –
The arterial steal syndrome is an uncommon but highly morbid complication of the vascular access necessary for hemodialysis. Presents as Pale/blue and/or cold hand without pain/or pain during exercise and/or hemodialysis, ischemic pain at rest, ulceration, necrosis and gangrene.
8. Uremic stomatitis-
It clinically represents as white plaques distributed predominantly on the buccal mucosa, floor of the mouth and tongue(6).It is considered as the reaction to a tissue irritant, possibly ammonia compounds derived from urea hydrolysis by salivary urease, whenever salivary urea level exceeds 180gm/dl. Treatment with a mildly acidic mouth rinse, such as diluted hydrogen peroxide clears oral lesionsUremic stomatitis
Conclusion:
Skin manifestations are fairly common and troublesome to patients affected by chronic renal failure. They negatively affect the quality of life of these patients causing constant worry in health care team. Therefore it is essential to identify and treat these diseases at the earliest.
References-
- Johnson AC, Leway AS, Coresh J, Levin A, Lau J, Eknoyan G: Clinical practical guidelines for Chronic Kidney Disease in adults: Part I. Definition, Disease stages, Evaluation, Treatment, and Risk factors. American Family Physician 2004;70:869-876.
- Prabahar MR, Chandrasekaran V, Soundararajan P. Epidemic of chronic kidney disease in India—what can be done? Saudi J Kidney Dis Transpl 2008;19:847-53.
- Udayakumar P, BalasubramanianS,Ramalingam KS et al. Cutaneous manifestationsin patients with chronic renal failure onhemodialysis. Indian J DermatolVenereolLeprol2006; 72: 119-25.
- Maurice PDL. Acquired perforating dermatosisin renal patients.Nephrol Dial Transplant.1997;12:2774-5.
- Lynde CB, Pratt MD. Acquired perforating dermatosis: association withLynde CB, Pratt MD. Acquired perforating dermatosis: association with diabetesand renal failure.CMAJ. 2009;181:615
- Neville BW, Damm DD, Allen CM. Oral manifestation of systemic diseases. In: Bouquot JE (Ed). Oral and Maxillofacial Pathology (2nd ed). USA: WB Saunders Company 2002:705-36