Introduction:
The use of a dermatoscope in clinical practice has been shown to increase diagnostic accuracy and is considered the standard of care in assessing patients with pigmented skin lesions. Its use is also being increasingly applied to the diagnosis of nonpigmented skin lesions. Dermoscopy has been shown to facilitate the clinical recognition of several inflammatory and infectious diseases, as well as their discrimination from skin tumours.With new evidence continuously being gathered, the dermatoscope gradually acquires a role similar to the stethoscope of general practitioners, becoming an irreplaceable clinical tool for dermatologists Application of dermoscopy should follow the standard procedure of acquiring information from patient history and clinically evaluating the number, location and morphology of the lesion(s).
Four parameters should be assessed when applying dermoscopy in the realm of inflammatory and infectious diseases:
- morphological vascular patterns;
- arrangement of vascular structures;
- colours; and
- follicular abnormalities,
while the presence of other specific features (clues) should also be evaluated.
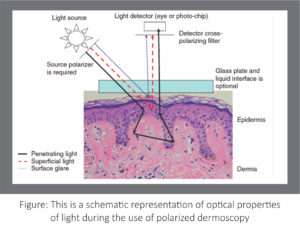

Figure: Difference between nonpolarized and polarized Dermatoscopy.
How do I interpret the dermatoscopic image?
There are only five basic elements used to describe pigmented structures, which are objectively defined using the following geometric terms (Figure 1):
- line: a two dimensional continuous object with length greatly exceeding width
- pseudopod: a line with a bulbous end
- circle: a curved line equidistant from a central point
- clod: any well circumscribed, solid object larger than a dot; clods may take any shape
- dot: an object too small to have a discernable shape. Lines are further classified into five types: reticular, branched, parallel, radial and curved, as these have diagnostic significance.

Figure : Structures seen
with a dermatoscope lines (A), pseudopods (B), circles (C) clods (D), dots (E), Lines can be reticular (F), branched (G), parallel (H) radial (I), Curved (J)
Blood vessels are also described using similar well defined Terminology. (Figure).
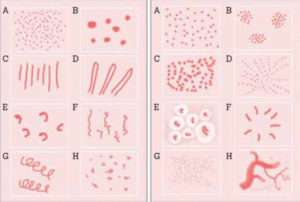
Figure. Vessel patterns :
Vessel Structure (left): dots (A) clods (B), lines (C), looped (D), curved (E),serpentine
(F), helical (G), coiled (H)
Vessel arrangement (right): random
(A), clustered (B), serpiginous (C), linear (D),centred (E), radial (F) reticular (G), branched (H)
Colour has great diagnostic significance in dermatoscopy. The main pigments are melanin and haemoglobin, and the colours produced are shown in Figure 3. Although melanin is black, it appears as different colours depending on how deeply in the skin it is located.Very superficially it looks black, but deeper in the epidermis it appears brown. In the dermis, melanin appears either grey or blue. Therefore in many circumstances, these colours indicate the presence of melanin pigment deeper in the
skin than expected, which can be a clue to invasive malignancy.
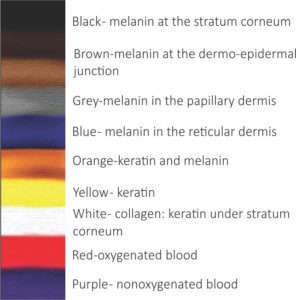
Figure. The interpretation of colours seen with a dermatoscope
Features of Dermatoscopy in Inflammatory and non-inflammatory diseases.
Papulosquamous dermatoses:
Lichen planus;
Dermoscopy enables the visualization of Wickham striae
(WS), which have been assessed as a highly sensitive and specific criterion for the diagnosis of lichen planus (LP).Wickham striae are seen as round, linear, reticular or annular pearly-whitish structures and may develop thin or broadarboriform projections, surrounded by dotted or linear vessels that highlight them.
Psoriasis;
Dermoscopy of plaque psoriasis (PP) typically reveals white scales and regularly distributed, dotted vessels on a light red background ( 2b and 3a). Detection of other morphological types of vessel should raise doubts about the diagnosis of PP.
Under higher magnifications (100–400), the psoriatic vessels appear as convoluted loops, mirroring the underlying histopathological finding of spiralled capillaries within the dermal papillae, associated with the psoriasiform epidermal hyperplasia.10 Although present in every psoriatic plaque, red dots are not a specific dermoscopic feature, as they can also be found in other papulosquamous dermatoses. Instead, their uniform, symmetrical, regular distribution throughout the lesion typifies PP. When an intense hyperkeratosis impedes the visualization of underlying structures, scale removal will bring to light the aforementioned vascular pattern, possibly together with tiny red blood drops (the dermoscopic ‘Auspitz sign’). Other patterns of vessel distribution are extremely rare in PP, with the exception of the highly specific, but relatively uncommon, pattern of ‘red globular rings’.
Dermatitis
Dotted vessels in a patchy distribution and yellow serocrusts represent the main dermoscopic criteria in all subtypes of dermatitis (Figs ). Depending mainly on disease duration, dermatitis may dermoscopically display a spectrum of scaling and vascular changes, with acute exudative lesions predominantly exhibiting yellow scale crusts (‘yellow clod sign’), whereas more chronic and lichenified lesions are typified mainly by dotted vessels in a patchy distribution within the lesion.
Pityriasisrosea:
Both the herald patch and the secondary lesions of pityriasis roseadermoscopically display peripheral whitish scales (‘collarette sign’), typically combined with dotted vessels that lack the regular distribution of psoriasis.

Lichen planus (a) may share clinical features with other papulosquamous skin diseases, such as dermatitis (c). However, dermoscopic detection of Wickham striae (b, arrows) allows a safe diagnosis of lichen planus, while dermatitis (d) typically shows dotted vessels with a patchy distribution and yellow scale crusts (arrows).
Dermoscopic differentiation between psoriasis and dermatitis;
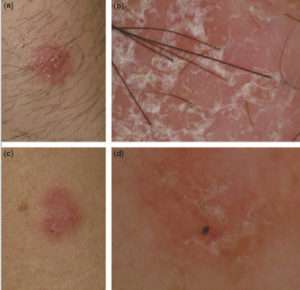
Dermoscopic differentiation between psoriasis (a, b) and dermatitis (c, d) is enabled by recognition of the white scales of the former in contrast to the yellow serocrusts of the latter.
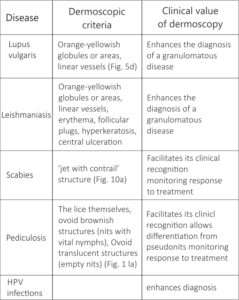
Dermatoscopic criteria for inflammatory skin diseases.

Dermatoscopic findings of Infectious skin disease:

Dermatoscopic finding in Hair disorders:
Alopecia Areata: yellow dots, black dots, exclamation mark hairs, and vellus hairs.
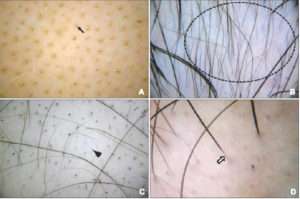
Figure: Dermoscopic features of alopecia areata; yellow dots (A; arrow), clustered vellus hairs (B; dotted circle), black dots (C; triangle), and tapering hairs (D; white arrow).
Dermatoscopic finidngs in tineacapitis:
Comma hairs, cadaverized hairs, coiled hairs, haemorrhagic spots, honeycomb pigment network, yellow and black dots, thin hairs , corkscrew hairs, broken hairs, peripilar scaling etc.
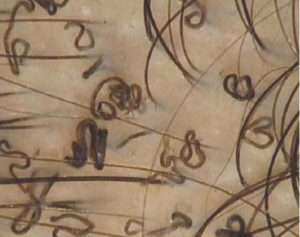
Figure: Video demoscopy 40x.comma and corkscrew hair in tineacapitis.
Three point check list in pigmented lesion to detect early melanoma:
The dermoscopy, 3-point checklist for early detection of skin cancer is fairly easy to learn and has a high sensitivity for melanoma. There a high likelihood of malignancy (melanoma or basal cell carcinoma) if a pigmented skin lesion has any two of these criteria. The 3-point checklist has been designed to allow non-experts not to miss detection of melanomas.
- Asymmetry: asymmetry of colour and structure in one or two perpendicular axes
- Atypical network: pigment network with irregular holes and thick lines
- Blue-white structures: any type of blue and/or white colour, i.e. combination of blue-white veil and regression structures.
Dermatoscopes and dermatoscopy
A dermatoscope is more than a magnifying lens and light source. By eliminating reflection from the skin surface, the dermatoscope allows better visualisation of the patterns formed by pigment and blood vessels – critical features in the diagnosis of skin lesions. This can be done using fluid to couple the lens to the skin or by cross-polarisation of light source and lens. Colour rendition varies with the different types of instruments,9 hence familiarity with your chosen device is important.
Conclusion
In summary, dermoscopy improves the clinical recognition of several inflammatory and infectious dermatoses, by enhancing the most basic of diagnostic functions in dermatology: visual the dermatoscope gradually acquires a role similar to the stethoscope of general practitioners, becoming an irreplaceable
clinical tool for dermatologists inspection.






