Deoxycholic acid is a bile acid formed by bacterial action from cholate. Bile acids are also steroidal amphipathic molecules derived from the catabolism of cholesterol. Bile acids are physiological detergents that facilitate excretion, absorption, and transport of fats and sterols in the intestine and liver. The unique detergent properties of bile acids are essential for the digestion and intestinal absorption of hydrophobic nutrients. Bile acids have potent toxic properties (e.g., membrane disruption) and there are a plethora of mechanisms to limit their accumulation in blood and tissues.
Deoxycholic acid acts as a detergent to emulsify and solubilize fats for intestinal absorption, is reabsorbed itself, and is used as a choleretic and detergent. When injected subcutaneously, it disrupts cell membranes in adipocytes and destroys fat cells in that tissue. In April 2015, deoxycholic acid was approved by the FDA for the treatment submental fat to improve aesthetic appearance and reduce facial fullness or convexity, allowing for a safer and less invasive alternative than surgical procedures.
It is rapidly absorbed following SC injection, peak plasma time being 18 minutes.
Deoxycholic acid is excreted along with the endogenous deoxycholic acid in the feces with levels return to the endogenous range within 24 hours.
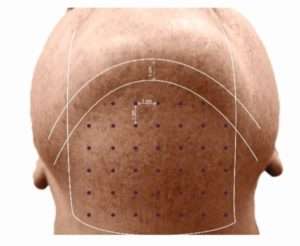
Deoxycholic acid is injected into subcutaneous fat tissue in the submental area using an insulin syringe, 30G needle and 13 mm of length. The needle should be held tangential to the skin or the skin needs to be pinched away from the underlying structures before injecting. The treatment is divided into points spaced 1 cm apart and 0.1 to 0.2 ml of the medicine is used in each point. The number of points depends upon the area and fat content. Up to 5 to 10 ml may be used in a given session. The number of sessions depends upon the extent of double chin but the treatment should only be repeated a month apart. Use of Deoxycholic acid outside the submental region has not been established and is not recommended.
Injections cause edema at injection sites, pain, erythema, induration and pruritus and may also cause hematoma, numbness, paresthesia nodule or ulceration (intradermal injection) in rare circumstances.
Presence of infection at the injection site or pre-existing dysphagia is a strong deterrent for the treatment. Patients shouldn’t be on anticoagulants or have bleeding abnormalities. Do not inject above the inferior border of the mandible. Do not inject within a region defined by a 1- to 1.5-cm line below the inferior border (from the angle of the mandible to the mentum). Avoid injection into the platysma. Prior to each treatment session, palpate the submental area to ensure sufficient submental fat. Use of ice/cold packs, topical and/or injectable local anaesthesia (eg, lidocaine) may enhance patient comfort.
Patients with excessive skin laxity may not appreciate the results unless the laxity isn’t addressed. Such patients should be adequately counselled about the same. Radio frequency or thread lifting can be done for such patients.
Photographs courtesy Geosmatic C & C

*-*-*