Introduction:
Acne Scars are the troublesome manifestation following acne, causing depression, social outcast, and most importantly cosmetic discomfort. They commonly affect those areas which are rich in pilosebaceous glands like face, back and shoulder. Genetic factors, disease severity and delay in treatment are the main factors influencing scar formation. A British study showed that 1% of the population reported having acne scars, 14% of which thought their scars to be disfiguring.
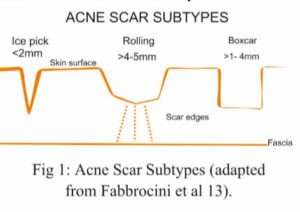
The acne scars are broadly classified as macular, atrophic & hypertrophic or keloidal scars. Atrophic acne scar are further divided into Ice Pick, Box, and Rolling Scars. Atrophic acne scars are more common than keloids and hypertrophic scars with a ratio 3: 1. The ice pick type represented 60%–70% of total scars, the box scar 20%–30%, and rolling scars 15%–25% in one clinical trial. Hypertrophic scars are typically raised and firm scars that remain within the borders of the original site of injury. In contrast, keloid scars form as reddish-purple papules and nodules that extend beyond the borders of the original wound.
Scar classification is important as it can help guide treatment options. Ice pick scars can extend deep into the dermis, which makes them resistant to conventional skin-resurfacing options. Rolling scars are wider and have fibrous anchoring to the subcutis, thus necessitating treatment at a subdermal level. Shallow boxcar scars are more amenable to skin resurfacing treatments whereas deeper boxcar scars are more resistant to such superficial treatments.
Treatment options can be broadly categorised into energy-based and non-energy-based. Commonly used energy-based technologies include ablative and non-ablative lasers, fractional radiofrequency, intense pulsed light and plasma skin regeneration. Non-energy-based devices include subcision, (micro) dermabrasion, microneedling, dermal fillers and chemical peels.
Subcision:
It is a non-operative technique that involves a needle being inserted subcutaneously and handled in a fanning motion in order to untether the fibrous strands within the scar, and stimulate new connective tissue formation that will help elevate the depressed surface of scars.
The treatment of post-acne scarring with subcision was assessed in many studies. The scars treated were mainly of the rolling type, with some studies including a combination of the other types. In a few papers, subcision was used in isolation; in one it was used in conjunction with subsequent suctioning; in one with either dermaroller or cryoroller application; in one with 15% trichloroacetic acid (TCA) peel; and in one study with 50% TCA peel. TCA Cross technique followed by subcision is also recommended for Ice pick scar.
In a randomised split-face study of ten patients, the effects of subcision with an 18-gauge Nokor needle were compared with those of collagen fillers in the treatment of different types of depressed acne scars. Assessment at six month follow-up for global improvement was graded as 2.95 and 3.05 and mean patient rating as 3.9 and 2.9 for subcision and fillers, respectively.1
Another study reported the results of a novel technique that included subcision with subsequent suctioning for a two-week period. They treated patients using mainly 23-gauge needles and applying suctioning with the hand piece of a MDA (Micro dermabression) device. The aim behind suctioning was the avoidance of scar re-depression. In patients with subcision and suctioning they observed a 60–90% scar improvement in respect to only 30-60% improvement among patients treated without subcision alone.2
A split-face study on 30 patients with multiple types of acne scarring assessed subcision followed by dermaroller on one side and subcision followed by cryoroller on the other. On the subcision and cryoroller side, mean percentage improvement was documented as 57% while, on the subcision and dermaroller side, mean percentage improvement was 40%.3
Subcision is one of the best treatments for acne scars. It is an outpatient department procedure, which is quick, cost effective and highly efficacious in acne scar management. It can be combined with other non-energy or energy based treatments to increase final outcomes. Yet a few adverse effects may occur like bruising, bleeding and acne flare up. Pre-treatment with Vitamin K, antiseptic cleaning and post treatment antibiotics may minimise the adverse effects.
Dermabrasion and microdermabrasion:
Dermabrasion (DA) and microdermabrasion (MDA) are facial-resurfacing techniques that mechanically ablate damaged skin in order to promote re-epithelialisation. DA completely removes the epidermis and penetrates to the level of the papillary or reticular dermis, while MDA is a much more superficial treatment and only removes the stratum corneum, accelerating the natural process of exfoliation.
In a study, patients with moderate to severe post-acne atrophic scarring of various types underwent a series of eight weekly treatment sessions. They used suction powers in the range of 40–60 kpa and four to six passes in each direction were performed (directed horizontally, vertically and obliquely). The average treatment lasted approximately 15 min. Following eight sessions of MDA, 27.3% patients achieved no improvement, 45.4% mild improvement, 18.2% moderate improvement and 9.1% good improvement. No patients were found to have achieved very good improvement in scar appearance.4
MDA alone is not a promising technique for the treatment of acne scars. It could be used to treat all kind of scars to a limited extent and I propose to combine it with other existing treatment options.
Microneedling:
Microneedling has become an important treatment modality for atrophic acne scars. The principle of using microneedling is to initiate collagen induction. This is achieved by causing minute injury to the dermis with the use of micro needles.
In a few papers, microneedling was used in isolation, in one it was compared with glycolic acid (GA) peeling and in another it was used in conjunction with platelet-rich plasma (PRP).
A split-face study was done to access the effects of microneedling with PRP versus microneedling with vitamin C application. Result shows better response in patients treated with PRP compared with patients who received treatment with vitamin C.5
Another study compared the effects of PRP versus the CROSS peeling technique with 100% TCA versus combined microneedling and PRP in the treatment of atrophic acne scars. There was no statistically significant difference in the degree of improvement between all the treatments.6
Microneedling is considered equivalent to energy based treatments and it is best when it comes to treat rolling scars, while in other types of scars combination techniques should be preferred. There are a few adverse effects associated with microneedling like Post Inflammatory Hyperpigmentation, acne flare up, bruising, or milia formation. All adverse effects are usually transient and wouldn’t require stoppage to the treatment.
Platelet Rich Plasma
Platelet rich plasma had been used successfully in wound healing in several studies. Higher amount of platelet derived growth factors make it suitable to use in several other indications such as treatment of androgenic alopecia, acne scar, graft survival in hair transplantation, skin rejuvenation, better wound healing, face lifting and several other cosmetic procedures.
In our split-face study with 50 patients, the effects of microneedling along with topical application and intradermal injections of PRP were compared with those of microneedling and intradermal administration of distilled water. After treatment, PRP treated patients showed 62.20% improvement in acne scars and 45.84% improvement of acne scars in patients treated with microneedling with distilled water.7
Platelet rich plasma contains several growth factors needed for proper wound healing and collagen induction. It could be combined with both energy based or non energy based treatments. PRP alone is not effective and is not worth trying, and should always be used in combination. Autologus PRP is cost effective, easy, and safe to treat acne scars without much adverse effects.

Fig A. 24 years female treated with three sessions of PRP with Microneedling
Dermal fillers:
Dermal fillers involve the injection of foreign body gels into the dermal or subdermal tissue in order to provide localised volume gain. A few studies assessed the effects of dermal fillers, mainly in patients with rolling type scars. One can utilise poly-L-lactic acid (PLLA), collagen, polymethyl methacrylate (PMMA) and hyaluronic acid (HA).
In one study, patients with severe scarring from acne or varicella treated with injectable PLLA fillers. They achieved a maximum cumulative scar severity reduction of 46.4% at the seventh treatment visit.8
Another study assessed the effects of PMMA versus placebo for the treatment of atrophic rolling acne scars. The overall proportion of scars that improved by at least two points was 50% for PMMA and 21% for the control.9
In a different study, PLLA fillers were used to treat 22 participants with facial rolling scars. A satisfactory response was achieved in 63.6% of patients when assessed by physicians, 68.2% when assessed by blinded evaluators and 45.5% when assessed by the patients themselves.10
Fillers are still having a limited role in the acne scar management as most of them used are not long lasting, expensive. Though fat grafting could help in some cases, still durability is in question here. Adverse effects associated with fillers also make them less useful in acne scars management.
Chemical Peeling:
Chemical peeling is the process of applying chemicals to the skin in order to destroy the outer damaged layers, thus accelerating the normal process of exfoliation, leading to tissue remodelling, thereby decreasing scar appearance.
In a study, patients with post-acne scarring were treated using a modified phenol deep peel. Results were assessed using a four-point scale. 64% patients improved by 51% or more.11
In another study, ten patients were treated using 100% with the TCA CROSS technique. The improvement was assessed using a four-point scale and results were interpreted as excellent if >70% reduction was observed, good if 50–70%, fair if 30–50% and poor if <30% improvement was observed.
A comparative study between Jessner’s peel and 20% TCA versus 20% TCA peel in isolation was done. Results showed no significant difference in improvement among both the peels.12
Conclusion:
Post-acne scarring is a very common and challenging condition with no easy and definitive solution. Subcision, microneedling, MDA, dermal fillers and chemical peels have all been used with varying degrees of efficacy but an overall positive outcome. Each technique has pros and cons. Some are suited for specific types of scars, others need to be applied repeatedly, and all carry a potential risk of adverse reactions.
References
- Sage RJ, Lopiccolo MC, Liu A, et al. Subcuticular incision versus naturally sourced porcine collagen filler for acne scars: a randomized split-face comparison. Dermatol Surg 2011; 37: 426–431.
- Harandi SA, Balighi K, Lajevardi V, et al. Subcision-suction method: a new successful combination therapy in treatment of atrophic acne scars and other depressed scars. J Eur AcadDermatol Venereol 2011; 25: 92–99.
- Gadkari R and Nayak C. A split-face comparative study to evaluate efficacy of combined subcision and dermaroller against combined subcision and cryoroller in treatment of acne scars. J Cosmet Dermatol 2014; 13: 38–43.
- El-Domyati M, Hosam W, Abdel-Azim E, et al. Microdermabrasion: a clinical, histometric, and histopathologic study. J Cosmet Dermatol 2016; 15: 503–513.
- Chawla S. Split face comparative study of microneedling with PRP versus microneedling with vitamin C in treating atrophic post acne scars. J Cutan Aesthet Surg 2014; 7: 209–212.
- Nofal E, Helmy A, Nofal A, et al. Platelet-rich plasma versus CROSS technique with 100% trichloroacetic acid versus combined skin needling and platelet rich plasma in the treatment of atrophic acne scars: a comparative study. Dermatol Surg 2014; 40: 864–873.
- Asif M, Kanodia S and Singh K. Combined autologous platelet- rich plasma with microneedling verses microneedling with distilled water in the treatment of atrophic acne scars: a concurrent split-face study. J Cosmet Dermatol 2016; 15: 434–443.
- Beer K. A single-center, open-label study on the use of injectable poly-L-lactic acid for the treatment of moderate to severe scarring from acne or varicella. Dermatol Surg 2007; 33 (Suppl. 2): S159–167.
- Karnik J, Baumann L, Bruce S, et al. A double-blind, randomized, multicenter, controlled trial of suspended polymethylmethacrylate microspheres for the correction of atrophic facial acne scars. J Am Acad Dermatol 2014; 71: 77–83.
- Sapra S, Stewart JA, Mraud K, et al. A Canadian study of the use of poly-L-lactic acid dermal implant for the treatment of hill and valley acne scarring. Dermatol Surg 2015; 41: 587–594.
- Park JH, Choi YD, Kim SW, et al. Effectiveness of modified phenol peel (Exoderm) on facial wrinkles, acne scars and other skin problems of Asian patients. J Dermatol 2007; 34: 17–24.
- Puri N. Efficacy of modified Jessner’s peel and 20% TCA versus 20% TCA peel alone for the treatment of acne scars. JCutan Aesthet Surg 2015; 8: 42–45.
- Fabbrocini G, Annunziata MC, D’Arco V, et al. Acne scars: pathogenesis, classification and treatment. Dermatol Res Pract2010; 2010: 893080.






