Introduction
The term “dermoscopy,” first coined by Friedman is also known as dermatoscopy, epiluminescence microscopy, or surface microscopy. It is a simple, noninvasive and practical technique in which a dermoscope, a handheld device with 10x magnification, is used to examine skin. Aptly called as “The dermatologist’s stethoscope”, it is a relatively young, dynamic and exciting field. 1It allows rapid in vivo evaluation of morphologic structures of epidermis, dermoepidermal junction and papillary dermis which cannot be seen by naked eye.3,4 Since the dermoscopic structures correlate well with the histopathologic alterations, dermoscopy represents an interface between clinical and histopathological findings.1,3
Historical aspects
Dermoscopy was first introduced for evaluation of pigmented / non-pigmented skin tumors. Earlier dermatoscopes used in late 1980’s were large devices that required an oil or alcohol interface to reduce light reflection, later in 1990s hand-held devices started being used. 2
Principle of dermatoscope
When a skin lesion is visualized with a magnifying loupe with lighting, most of the light is scattered due to reflective property of stratum corneum. In order to allow more light to pass through stratum corneum, to enable deeper visualization of pigment and vascular patterns, two ways can be used. One is by using a fluid medium as an interface and a transparent glass contact plate and the other is by using a cross polarized light.The newer dermoscopes are provided polarized light allowing both contact and noncontact dermoscopy.2
Dermatoscopes available
- Handheld polarized dermoscopes
They are highly portable with magnification of 10 to 20 X, do not require skin contact or immersion fluid and allow rapid and safe examination without the risk of possible transfection .3,4These devices can distort colors, so they also have contact dermoscopy capabilities to minimize color distortions.1 They can be used to take photographs by connecting them with cameras, smart phone cameras and digital SLRs, using adapters.2 Figure 1 shows a hand held dermatoscope.

- Nonpolarised light contact dermoscopy
In contact dermoscopy, the device emits a beam of light which strikes the skin at a 20º angle. To eliminate reflections and thus enable better visualization, a fluid like oil, water, gel, glycerin, or ethanol gel is placed between the skin and the device.1 These devices are not preferred as they may reduce the vessels (due to pressure) and/or scaling (when using a liquid interface) visibility, but some superficial findings like comedo-like structures, milia-like cysts and crypts (seen in seborrheic dermatitis) and the blue-white veil seen in melanoma are better seen with these devices.5 Disposable contact caps, food wraps, adhesive tapes, and 70% ethanol (as interface fluid) help to avoid cross infection in contact dermoscopy.2
- Video dermoscopes
These devices need to be connected to a viewing monitor, usually with a USB connection. Advantages are that a larger view is obtained which can be shared with the patients/ dermatologists and images can be stored. These devices are expensive and are usually restricted to research centers.2
- Multispectral dermoscopes and UV dermoscopes
These allow better visualization of specific structures eg surface pigmentation is better seen under blue light, superficial vascularity under yellow light and deeper pigmentation and vascularity with red light which penetrates deeper.2
A good quality hand-held, portable device with both contact dermoscopy and cross polarized light options can be considered best for a beginner.2
Uses of dermatoscope4,5
Dermoscopy is useful for diagnosis of common dermatologic diseases, especially in atypical/unusual cases. 3Various uses of dermoscopy include
1. Dermoscopy for pigmented and non-pigmented skin tumors including melanocytic/ non-melanocytic and benign/ malignant skin tumors.
a.Dermoscopy provides useful and reliable information on the histopathologic basal cell carcinoma (BCC) subtype, reveals tumor characteristics like ulceration or pigmentation, facilitating the accurate management of the tumor. Presence of ulcerations represents a predictor of favorable response to imiquimod. Dermoscopy reveals pigmentation in 30% of clinically non-pigmented BCCs, which is relevant for BCCs scheduled to be treated with photodynamic therapy (PDT), as pigmented tumors are less responsive to PDT.3
b.Dermoscopy allows accurate assessment of true extension of tumor, facilitating a more precise estimation of the required surgical margins, thus helping to minimize recurrence rates.3
c.Dermoscopy is useful for diagnosing different stages of keratinocyte skin cancer, thus improving the treatment.3
2. Inflammoscopy for various inflammatory diseases like psoriasis, lichen planus, pityriasis rosea etc.
Because of specific features on dermoscopy, the differential diagnosis of the papulosquamous disorders becomes simpler, permitting recognitation of lichen planus (Wickham striae), eczema (yellow crusts and patchy dotted vessels), and pityriasis rosea (peripheral white scales). The inflammatory dermatoses may be a major reason for use of dermatoscope given their incidence and the difficulties in their differential diagnosis.3
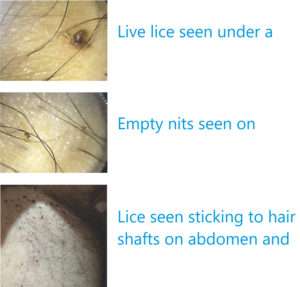
3. Entomodermoscopy for skin infections and infestations caused by parasites, viral, bacterial, fungal or protozoan infections.
Both common (warts, molluscum contagiosum, mycosis and mite infestations) and uncommon (myiasis and tinea nigra) infestations can be diagnosed by dermoscopy, scabies representing a good example showing the delta-wing jet with contrail.3
4. Trichoscopy for diagnosing hair and scalp disorders.
The term was coined by Rudnicka and Olszewska in 2006. Trichoscopy improves diagnostic accuracy and may help in better understanding of pathogenesis of hair disorders.6
5. Nail/nailfold abnormalities (Onychoscopy/ Capillaroscopy) 7
a.It may be useful for diagnosis of small, subclinical/ subungual warts or for the assessment of therapeutic response after treatment.Decrease of capillary density within viral warts is observed in lesions responding to treatment.
b.Dermatoscopy helps to localize tumors and to visualize vascular patterns. It facilitates the delimitation of surgical margins before treatment.
c.In subungual melanoma, the Hutchinson sign defined by the visibility of a pigmentation of the periungual cuticula, can be demonstrated by dermatoscopy.
d.Sequential digital dermatoscopy may help to detect dynamic changes in color and increase in width of whole longitudinal pigmentation over a period of time.
e.Nail fold capillaroscopy is useful for screening of autoimmune diseases. Presence of dilated capillaries and/or nail fold hemorrhage on dermatoscopy is a sensitive and specific for diagnosis of systemic sclerosis.
6. Other disorders
a.The detection of a yellow-orange background is considered a dermoscopic clue for the diagnosis of granulomatous skin disorders like sarcoidosis, lupus vulgaris.3
b.Dermoscopy has been found useful in the diagnosis of rosacea, discoid erythematous lupus, morphea, lichen sclerosus, pigmented purpuric diseases, Darier’s disease, Grover’s disease, porokeratosis etc.3
7. Dermoscopy for monitoring.
a.Utility of dermoscopy for therapeutic monitoring of imiquimod treatment has been reported.1
b.Dermatoscopy has been used to evaluate vitiligo activity. Balakrishna et al used dermatoscope to monitor the result of various surgical procedures in vitiligo.8
Criteria/factors to be considered while using dermoscopy2,5
The criteria include
- Morphology/arrangement of vascular structures
- Scaling patterns
- Colours
- Follicular abnormalities
- Specific features
The factors include
- Quality
- Budget
- Need for documentation
- Major types of cases one sees
Advantages of dermatoscopy 1
- It reduces the uncertainty of clinical examination, thus improving diagnostic accuracy.
- It enables detection of tumors at earlier stages, thus improving the prognosis.
- It reduces the need for unnecessary biopsies.
- It provides guidance on the optimal site for biopsy, thus improving the histopathological accuracy.
Studies on dermatoscopy
Scientific publications on dermoscopy have increased significantly with more than 1000 articles been published between 2003 and 2007.9 Criteria and dermoscopic patterns have been established for melanoma /melanocytic nevi, basal cell carcinoma, seborrheic keratosis, squamous cell carcinoma, Bowen’s disease and many more benign skin tumors. Trichoscopic criteria for localized and diffuse hair loss have also been described.2
International Dermoscopy Society
The International Dermoscopy Society (IDS) founded in 2003, promotes education and research, and conducts conferences and multicentre studies in the field of dermoscopy.2,9
Conclusion
Dermoscopy is an irreplaceable, noninvasive and helpful auxiliary tool in assisting the recognition/ differential diagnosis of various dermatoses, reflecting their histopathological background, thus having a great impact on clinical practice of dermatology.5Thus it is definitely worth the investment.
References
- Heliane Sanae Suzuki,Sérgio Zuñeda Serafini, Maurício Shigueru Sato. Utility of dermoscopy for demarcation of surgical margins in Mohs micrographic surgery.An Bras Dermatol. 2014 Jan-Feb; 89(1): 38- 43.
- Feroze Kaliyadan.The scope of the dermoscope. Indian Dermatol Online J. 2016 Sep-Oct; 7(5): 359–363.
- Teresa Russo, Vincenzo Piccolo,Aimilios Lallas, Giuseppe Argenziano. Recent advances in dermoscopy. Version 1. F1000Res. 2016; 5: F1000 Faculty Rev-184.
- Iris Zalaudek, Aimilios Lallas, Elvira Moscarella,, Caterina Longo, H. Peter Soyer, Giuseppe Argenziano. The dermatologist’s stethoscope- traditional and new applications of dermoscopy . Dermatol Pract Concept 2013;3(2):11
- Enzo Errichetti . Giuseppe Stinco. Dermoscopy in General Dermatology: A Practical Overview. Dermatol Ther (Heidelb) (2016) 6:471–507.
- Vivek V Nikam , Hita H Mehta.A Nonrandomized Study of Trichoscopy Patterns Using Nonpolarized (Contact) and Polarized (Noncontact) Dermatoscopy in Hair and Shaft Disorders. Int J Trichology. 2014 Apr-Jun; 6(2): 54–62.
- Holger A. Haenssle, Andreas Blum, Rainer Hofmann-Wellenhof, Juergen Kreusch, Wilhelm Stolz, Giuseppe Argenziano, Iris Zalaudek, Franziska Brehmer. When all you have is a dermatoscope-start looking at the nails. Dermatol Pract Concept 2014;4(4):2
- Balakrishnan Nirmal.Use of Dermatoscope to Monitor the Repigmentation of Various Vitiligo Surgical Procedures. J Cutan Aesthet Surg. 2016 Oct-Dec; 9(4): 286-287.
- Giuseppe Argenziano, Iris Zalaudek. Dermoscopy: a new perspective. Dermatol Pract Concept. 2011 Jan; 1(1): 57-58.