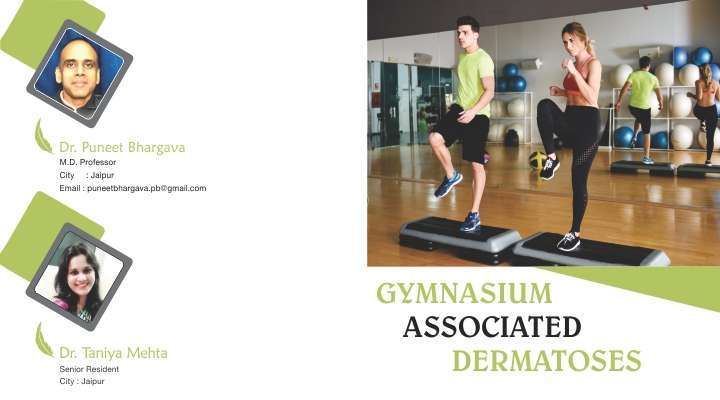
Exercise and sports are an integral part of almost everyone’s life especially since the notion of ‘Stay fit, Stay healthy’ seems to be the universal mantra. Unfortunately the benefits of exercise are often accompanied by multitude of unhealthy side effects. Sporting activities can led to a variety of infectious and non-infectious dermatoses. As a consequence sports dermatology is a budding field in which lots of work is being done. Gym is the ultimate destination for those who wish for fitness without having to step out and at any time of the day. As the summer approaches so rises the gym memberships and the skin ailments associated with it. The using of common handles, dumbbells, weights, common towels and baths can lead to a variety of infections. The trauma associated with vigorous exercises is another problem.
Infectious dermatoses
1. Bacterial:
(a) Folliculitis: MRSA and MSSA,
(b) Pitted keratolysis
2. Fungal:
(a) Tinea cruris and corporis
(b) Candidial intertrigo
(c ) Pityriasis versicolor and folliculitis
3. Viral:
(a) Molluscum contagiosum
(b) Verrucae
Non-infectious dermatoses
1. Trauma:
(a) Piezogenic pedal papules
(b) Callosity and corn
(c) Talon noir
(d) Jogger’s toe
(e) Friction blister
2. Striae distensae
3. Allergic/ irritant contact dermatitis : intertrigo, sweat dermatitis0;
4. Exacerbation of previous dermatoses
5. Urticaria and anaphylaxis
6. loose skin and wrinkling
FOLLICULITIS:
Defined histologically as presence of inflammatory cells in the hair follicle, it usually presents as follicular based pustule or abscess. If superficial, it is limited to the infundible of hair follicle and in deep folliculitis not only deeper portions of follicle are involved, it even extends to surrounding dermis. Deep folliculitis leading to abscess is called furuncle and multiple furuncles coalesce to form carbuncle. Community acquired skin and soft tissue infections (SSTI) are usually caused by staphylococci and streptococci.
Over the last few decades there has been an increase in Methicillin resistant Staphylococcoal aureus (MRSA) especially community acquired (CA-MRSA) in athletes and gymnasiums. Nagaraju et al reported isolation rates of 11.9% of CA-MRSA in India[1]. Another study in Pondicherry by Veniyill et al reported 17% isolation rate of CA-MRSA from cases of pyoderma[2].
CA-MRSA is more virulent than hospital associated MRSA and the resistance is due to SCCmec type IV gene sequence. The mecA gene produces transpeptidase PBP2a which decreases bacterial affinity for beta-lactam antibiotics. Besides this, SCCmecIV gene also codes for Panton Valentine Leucocidin (PVL) toxin.
Most CA-MRSA infections manifest as folliculitis and rarely joint pain. Gym associated CA-MRSA may present as an abscess with surrounding cellulitis in an athletic young adult with severe pain due to PVL activity. Rarely systemic dissemination may occur.
Transmission occurs via open wound, poor personal hygiene or hand washing, sharing personal items like towels, and improperly disinfected gym equipment.
TREATMENT AND MANAGEMENT:
1. Mupirocin and retapamulin can be used topically twice daily for 5 days on limited impetignised lesions and in nares for nasal carriers post nasal swabs and culture.
2. Oral regimens for outpatient settings are Bactrim-DS 1-2 tablets twice daily for 7 days, Clindamycin 300mg thrice daily, 100mg Doxycycline twice daily or Linezolid 600mg twice daily.
3.Inpatient treatment includes surgical debridement with intravenous antbiotics including Vancomycin 30mg/kg/day iv in 2 divided doses, Linezolid 600mg every 2 hours, Clindamycin 600mg every 8 hours, Daptomycin 4mg/kg i.v every 24 hours, Ceftaroline 600mg every 12 hours and Dalbavancin g iv once weekly.
4.Susceptibility test should be done according to local resistance rates and if patient fails to improve in 48 hours.
PREVENTION:
1. Open wounds should be covered and protected
2. Gym equipment should be properly disinfected periodically.
3.Personal items should not be exchanged.
4. Proper hand washing using liquid soap should be encouraged.
5. Early bathing post workout should be encouraged.
6. Actively infected persons should avoid gyms for 72 hours post start of antibiotics to decrease infection spread.
PITTED KERATOLYSIS (keratoma plantare sulcatum):
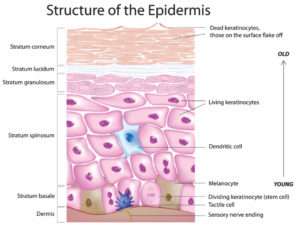
It is a superficial cutaneous bacterial infection characterised by crateriform pitting on pressure bearing areas of plantar surface of feet. Causative organism is Micrococcus sedentarius, Dermatophilus congolensis, Corynebacterium or Streptomycin species. Due to prolonged occlusion by shoes in gym coupled with sweating, bacteria proliferate and release proteinases that destroy stratum corneum and create the characteristic lesions. Associated malodor is due to thiol by-products of the bacteria.
FUNGAL INFECTIONS :
Due to prolonged sweating, maceration, exchange of personal items and infected surfaces cutaneous fungal infection like tinea, candidial intertrigo, pityriasis versicolor and follicultis may occur.
Pityrosporum (Malassezia) folliculitis: An inflammatory skin disorder caused by cutaneous flora Malassezia furfur in young adults. Disease presents as chronic, erythematous, pruritic follicular papules and pustules on back, chest and occasionally neck, shoulders, upper arms and face.
The organism is present in the ostium and deeper parts of hair follicle. Follicular plugging with yeast overgrowth in the presence of excess sebum leads to increased long- and medium-chain fatty acids which activate alternative complement and cell-mediated pathway.
Orally a course of ketoconazole, pulse itraconazole or weekly fluconazole can be given till lesions resolve. Topical treatment includes topical azoles especially ketoconazole, cicloprox olamine, Whitfield ointment and selenium sulphide shampoo for long period as relapses are very common.
PITYRIASIS / TINEA VERSICOLOR: A very common superficial mycoses, it is called
A very common superficial mycoses, it is called versicolor because it presents with hypopigmented, hyperpigmented and erythematous macules and patches on chest, back, upper arms and rarely face. The disease is characterised by cutaneous anergy specifically to Malassezia, a common commensal of skin. Fungi tends to invade the stratum corneum. Repeated recurrences are seen in predisposed patients.
The causative organism is Malassezia species (formerly called Pityrosporum) which includes M. furfur, M globosa, M sympodialis, M pachydermatis, M slooffiae, M. obtuse, M. restricta, M dermatis, M japonica, and M. yamatoensis. With adequate conditions like genetic predisposition, warm and humid climate, excess sweating and maceration the saprophytic yeast spores convert to parasitic mycelia forms. In recent years Malassezia has been implicated in a variety of other conditions like seborrheic dermatitis, acne, confluent and reticulate papillomatosis of Gougerot and Carteud, Psoriasis, Atopic dermatitis and BCC.
Effective topical treatment options are selenium sulfide, cicloprox olamine, azoles and allylamine antifungals. Oral recommended regimens are 200 mg/day itraconazole for 5-7 days, 400mg fluconazole weekly for 2 weeks or 200 mg/day for 2 days of Pramconazole. In recurrent cases, prophylactic treatment with monthly tablet of fluconazole or itraconazole may help. Frequent showers with change of clothes and avoidance of maceration helps. The disease is not contagious and pigmentary alterations too resolve within a few months.
DERMATOPHYTOSIS (TINEA):
A very common superficial cutaneous mycoses affecting the skin, hair and nails, that does not extend beyond epidermis. Based on species classified into tinea caused by Trichophyton, Epidermophyton and Microsporon Sp. Causative organisms can be anthrophilic (native to humans), zoophilic and geophilic, the latter two being the cause of inflammatory lesions. Based on topography, it can be tinea cruris, corporis, capitis, pedi, manum, barbae, faciei and unguim (onychomycoses). On morphology it can be tinea incognito, imbricata, pseudoimbricata and Majocchi’s granuloma. Sportspersons and people doing regular workouts tend to present with tinea cruris and corporis due to favorable fungal atmosphere like maceration, occlusion and sweating and onychomycoses, tinea pedis and manum and rarely candidial intertrigo due to old sweaty socks or long usage of occlusive footwear. Trichophyton rubrum is the
commonest species isolated from Rajasthan and Chennai while T. mentagrophytes is commonly isolated from northern India. Cell-mediated immunity is protective against dermatophytoses while humoral and innate immunity are not of much help.
Patient should be advised to wear loose-fitting cotton clothes, frequent change of undergarments and keeping the affected area dry. Counseling should be done to avoid sharing of personal items. Topical treatment includes Whitfield’s ointment, Castellani paint, topical azoles, allyl amines, amphotericin. For limited lesions simple topical therapy suffices for a period of 2-4 weeks and oral agents are needed for extensive, resistant lesions especially involving nails, palms and soles.
RECOMMENDED DOSING OF ORAL ANTIFUNGALS IN DERMATOPHYCOSES:

MOLLUSCUM CONTAGIOSUM (MC):
A cutaneous viral infection caused by pox virus, the disease presents as small pink to white umbilicated papules commonly on face, intertriginous areas and genitalia. Till date 4 viral strains have been isolated causing MC. In healthy young adults disease usually spreads by fomite transfer like infected gym equipment, infected floors and sharing of personal items like towels and soaps.
The incubation period is 3-6 weeks during which intra-cytoplasmic viral replication occurs forming inclusion bodies and causing enlargement of infected cells. The virus tends to be limited to the dermis. In 10% of cases molluscum dermatitis develops. The virus evades immunity by production of virus-specific proteins. Antibody production occurs but is not helpful, while CMI is protective.
The prognosis is excellent in healthy individuals, with even spontaneous resolution in few. The disease treatment can be done by a variety of methods. Topical treatment includes imquimod cream, cantharidin, tretinoin, TCA, salicylic-lactic acid, silver nitrate, topical cidofovir, rifampicin, podophyllin and potassium hydroxide. Curretage remains the most effective treatment in limited lesions. Cryotherapy and electrocautery can be done too. Intralesional interferon, autoinoculation have been tried in few studies. A sinecatechin Veregen, a green tea extract is being used off-label as 15% paste thrice daily.
VERRUCAE VULGARIS (WARTS):
warts are benign proliferation of the skin and mucosa caused by Human Papilloma Virus (HPV). Till date more than 100 types of HPV have been isolated. Virus tends to infect upper layers of epidermis and cause proliferation. Warts can plane, filirorm, anogenital, mucosal and palmoplantar. Sportsperson and athletes most frequently tend to develop palmoplantar and plane warts from sharing personal items and infected gym equipment. Disease spreads via fomite transfer, autoinoculation and virus enters by superficial abrasions. Incubation period is long usually 3-9 months and relapses and recurrences are frequent.HPV 16, 18, 9, 11, 30, 35 have oncogenic potential.
Common warts present as hyperkeratotic papules with irregular surface and varying sizes. Palmoplantar warts, also called as myrmecia are usually deep well-defined keratotic lesions with a callused periphery. They tend to be deep, painful, on weight bearing areas and resistant to treatment.
TREATMENT –
Topical agents used are 70% salicylic acid, salicylic-lactic acid combination, 5- fluorouracil, TCA, imiquimod, tretinoin, cantharidin, podophylln, contact sensitisers like diphencycloprenone and squaric acid dibutyl ester, aminolevulinic acid with blue light and cidofovir.
Intralesional bleomycin, interferon, candidial antigen, MMR or BCG vaccine have also shown success.
Resistant cases especially palmoplantar can be treated with liquid nitrogen cryotherapy, electrocautery, surgical paring and removal.
Veregen, a green tea sinecatechin extract as 15% paste thrice daily has been FDA approved for treatment of warts.
PDA with ALA and CO2 laser have been tried but their use and safety is debatable.
PIEZOGENIC PEDAL PAPULES:
Resulting due to herniation of fat via fascia into the dermis, these present as small tender firm and compressible papules on the sides of feet and occasionally wrist. Treatment includes wearing orthotic shoes, weight loss, avoidance of prolonged standing and analgesics but permanent relief is usually not achieved. Intralesional infiltration of bupivacaine with betamethasone has shown promise.
CALLOSITY AND CORN: Callus is a hyperkeratotic plaque on
Callus is a hyperkeratotic plaque on site of repetitive pressure, trauma or friction. It is one of the most common sport specific dermatoses. Corn is localised hyperkeratotic tender lesion with a central core on bony prominences. Treatment involves use of keratolytics, paring, pressure relieving orthotic shoes, radiofrequency removal and rarely surgical correction. Corns and calluses can be a very stubborn and physically handicapping disability and should be treated in conjunction with an orthopedic specialist and physiotherapist.
TALON NOIR:
Also called as black heel, it is caused by intra-epidermal haemorrhage over heel and calluses secondary to microtrauma of vasculature secondary to lateral shearing forces. It presents as black dyspigmentation over the affected area. Treatment includes reassurance, analgesics and paring, if required.
JOGGERS’S TOE (tennis toe):
Seen as subungual haematoma in treadmill runners precipitated by rapid starting or stopping, it needs to be differentiated from acral lentiginous melanoma. Reassurance is the key.
FRICTION BLISTER:
These occur due to repetitive shearing forces on opposing surfaces especially with new shoes or extensive use of dumbbells and weights. Presenting as fluid filled blisters of various sizes on both feet or hands, they can be prevented by using cushioned gloves, well fitting shoes and socks. Blisters can be punctured using sterile needle and topical antibiotic with rest of affected area for a couple of days help for healing.
STRIAE DISTENSAE:
Striae occur due to extensive stretching of elastic fibres thanks to sudden weight fluctuation or anabolic steroid usage and are commonly seen on back, arms and legs. Striae are extremely resistant to treatment. TCA application, topical tretinoin, microneedling, PRP and fractional CO2 and erbium-glass laser have been tried with varying rates of success.
SWEAT DERMATITIS:
This form of dermatitis was originally reported from western Rajasthan and is usually ignored or misdiagnosed. Associated with profuse sweating in summers, this disease presents with discolouration and roughening of skin to give a ‘charred appearance’ on trunk, neck and axillary folds. No obstruction of sweat glands is seen. Treatment includes application of mild topical corticosteroid lotions for a few days with oral antihistaminics[3].
URTICARIA AND ANAPHYLAXIS:
Cholinergic urticaria in the form of monomorphic itchy papules can occur due to workout induced sweating. Heat induced urticaria and angioedema can also rarely be precipitated by exercise. Exercise induced anaphylxis can occur in the susceptible especially if workout is done within an hour of food ingestion. Treatment includes antihistaminics, short course corticosteroids and leukotriene antagonists.
INTERTRIGO:
It is an inflammatory dermatoses of skin folds aggravated by friction, moisture, sweating and occlusion by tight clothes. Superinfection by candida most commonly, or bacteria can worsen the clinical picture. Clinically erythematous weeping lesions with satellite lesions and severe burning and itching is seen in crural folds, axilla and infra-mammary area. Lesionscan be relapsing and recurring. Irritant/ allergic dermatitis to synthetic gym wear and arm/ knee bands can also lead to eczematous lesions
Treatment needs to be tailored based on individual causes and keeping affected area dry .is the key. Inciting factors need to be avoided.
CONCLUSION:
Gym is a great avenue for not only staying fit but a social meeting place too. Given its communal nature, it plays host to a multitude of dermatoses, infectious and non-infectious. A dermatologist must keep his mind and eyes open for any clues to the above so that timely intervention can be done.
BASIC PREVENTIVE MEASURES
1.Take bath as soon as possible post workout.
2.Use of liquid handwashes and sanitisers during workout should be encouraged.
3. Use of well fitted and cushioned shoes with change of cotton absorbable socks daily.
4. Avoid sharing of personal products like towels.
5. Disinfect machine handles, weights and dumbbells regularly and use of cushioned cloves can be stressed upon.
6. Use of cotton gym wear.
SUGGESTED READINGS:
1. Nagaraju U, Bhat G, Kuruvila M, Pai GS, Jayalakshmi, Babu RP. Methicillin-resistant Staphylococcus aureus in community-acquired pyoderma. Int J Dermatol. 2004 Jun;43(6):412-4.
2. Venniyil PV, Ganguly S, Kuruvila S, Devi S. A study of community-associated methicillin-resistantStaphylococcus aureus in patients with pyoderma. Indian Dermatol Online J 2016;7:159-63
3. Mehta RD, Bumb RA. Sweat dermatitis. Int J Dermatol.2000 Nov;39(11):872.