- Dermatophyte infections encountered in day to day practice are on the rise
- Commonly used oral antifungal drugs fail to show response
- True prevalence difficult to determine because of self treatment / live with chronic infection
- Risk of acquiring such an infection is 10-20%
- Seen in all age groups & both genders
- Reasons for treatment failure are many
- True prevalence difficult to determine because of self treatment / live with chronic infection
- Poor adherence to treatment
- Re-infection from close contacts
Host factors responsible for recalcitrant nature of infections
- Non compliance or non adherence of schedule
- Inadequate dosing
- Use of tight synthetic, occlusive clothing
- Co morbid situation – Diabetes, Obesity, Anemia
- Immunocompromised states, atopy, thyroid
- High risk profession – cooks and domestic help
- Missed tinea of vellus hair on glabrous skin
- Hidden tineaunguim
Parasitism of the hair could be the cause of the majority of isolated lesions of ringworm of hairless skin with a poor outcome with topical antifungal treatment
In some patients, some short thin hairs fell easily on to the slide during the skin scraping. On microscopy, all the few vellus hairs identified in direct examination were affected.
Excoriation may also play a role in the development of tinea of the vellus hair, probably due to scratching, making some dermatophytes located in the stratum corneum penetrate into the hair follicle.
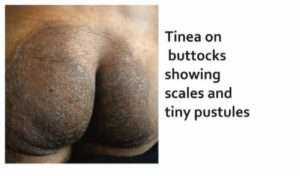
Diagnostic clues in tinea of vellus hair
- Inflammatory and/or excoriated lesions of tineacorporis or faciei
- Follicular micropustules
- Previous use of topical corticosteroids
- Resistance to topical antifungal treatment
- Falling of short and fine hairs to slide by scraping
Parasitism endothrix/ectothrix under potassium hydroxide examination
Reference:
- Mukherjee Pranab K. et al – Clinical Trichophytonrubrum Strain Exhibiting Primary Resistance to Terbinafine. Antimicrobial agents and Chemotherapy 2003 Jan; 47(1): 82–86
- Diagnostic Value of selected signs and symptoms in tinea infection. AFP 1998 Jul 1;58(1): 163-174
- Turnidge J, Paterson DL. Setting and revising antibacterial susceptibility breakpoints. ClinMicrobiol Rev. 2007;20:391-408
- Clinical Infectious Diseases 2008; 46:120–8
- British Journal of Dermatology 2010 163, pp603–606






